The MAA Hub-Spokes Model
The MAA Hub-Spokes Model
The Maternal Aid Association (MAA) has devised a primary healthcare model to revolutionise maternal healthcare in rural Bangladesh.



The Maternal Aid Association (MAA) has devised a primary healthcare model to revolutionise maternal healthcare in rural Bangladesh.



The Maternal Aid Association (MAA) has devised a primary healthcare model to revolutionise maternal healthcare in rural Bangladesh. This is known as the Hub-Spokes (HS) model. The HS model has been designed to educate a population, specialise the workforce and connect rural communities to a healthcare system. The main aims are to bring together a fragmented health system; access the remote and resource-poor populations, and add practical innovation and essential targeted resources to the field. To achieve this, MAA aims to reduce the delays pregnant women experience in a) deciding to seek care, b) reaching care and c) receiving adequate healthcare, as highlighted in the Three-delay model. Through targeting these areas, MAA aims to improve maternal health outcomes and ultimately allow the HS to serve as a blueprint for a model that can be replicated throughout the developing world, in similar resource-poor and remote settings. MAA will be piloting this model in March 2020 in Moulvibazaar, Bangladesh. The project will be overseen by Prof. Quazi Monirul Islam (LSHTM) and Dr. Ed Fottrell (UCL), MAA’s academic advisors in the UK as well as the Royal College of Obstetrics & Gynaecology (RCOG) in Bangladesh.
There are three main aspects of the model
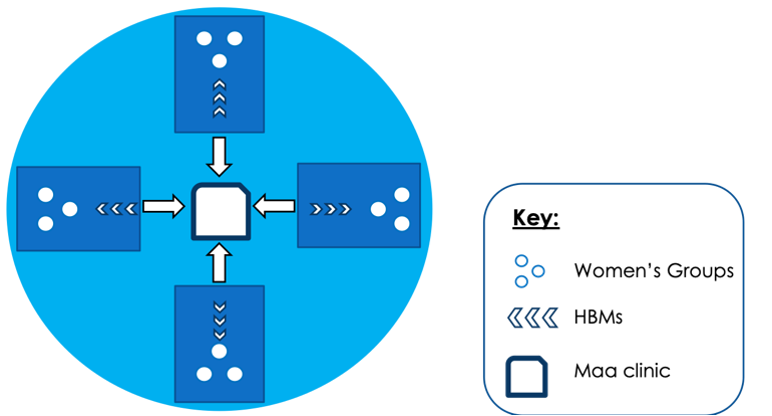
Figure 1: The Hub-Spokes Model. There are three main aspects to the model: Women’s Groups, Health Brigade Members, and the MAA Clinic with its specialised doctors. The MaaConnect app will be used to bridge the technological gap between the different components of this model.
Women’s Groups are a community-based intervention connected within the HS model. This is where local women will meet fortnightly to be educated on maternal and general health, providing a safe space for discussion and raising issues. They will be led by a trained and equipped facilitator, who will follow the Participatory Learning and Action cycle that enables women to play an active and influential part in decisions which affect their lives. MAA hopes that through these women’s groups, women will develop positive health-seeking behaviours and practices during pregnancy, labour and the postnatal period, and this will, in turn, decrease the maternal and neonatal mortality rate in Bangladesh. Professor Kishwar Azad (UCL) is the MAA academic advisor who will be responsible for implementing Women’s Groups in the villages. Women’s Groups have proven to be successful in reducing maternal and neonatal mortality previously, but MAA’s HS model will develop this intervention further by connecting the project to a primary healthcare system. MAA hopes these groups will educate and empower a generation of women, and address the delay in deciding to seek care by encouraging women to be more proactive in, and receptive to receiving healthcare.
Health Brigade Members (HBMs) are the next community intervention deployed in the HS model acting as our pivotal ‘spokes’. They are 5th year medical students (from MAA’s five affiliate medical schools in Bangladesh) on their Community Medicine placement. HBMs will provide antenatal care (ANC), screening and advice in the homes of pregnant women. They will also collect data on maternal and neonatal health outcomes, as well as demographic information for vital future research by MAA. They will be responsible for referring high-risk pregnancies to the MAA clinic for closer review by the specialised doctors. The HBMs responsibilities include recording and interpreting observations, educating and informing pregnant women, and identifying and referring high-risk pregnancies through the MaaConnect app. This addresses the delay in receiving healthcare as women will be accessing primary healthcare through a more efficient referral system. Through the HBM component of the HS model, MAA also aims to shift the mindset of future doctors in Bangladesh by training them to recognise the importance of equality in healthcare and encouraging them to consider working in rural settings.
Finally, the MAA clinic acts as the ‘hub’; it is an external clinic that will be utilised by MAA’s specialised doctors. These are foundation level doctors who will complete an intensive training programme, delivered by the Royal College of Obstetrics and Gynaecologists (RCOG) in Bangladesh and recognised by the RCOG UK. The primary role of MAA doctors in the HS model is to identify, manage and/or refer high-risk pregnancy cases. They will provide comprehensive antenatal care (ANC) at the clinic on a fortnightly basis to high-risk women, some of whom may have been referred by HBMs. They are the only healthcare workers in the model who can prescribe medication to patients when needed. By continuously monitoring women during pregnancy, the doctors are able to identify those who need to be rapidly referred to a hospital for secondary and tertiary level care. In the time lag between recognising the emergency and arranging transport, the doctors provide short term solutions such as the administration of Misoprostol, to reduce the risk of death by postpartum haemorrhage. The MAA clinic is therefore essential in the delivery of adequate healthcare and also facilitates the referral and transportation of women to secondary or tertiary health centres, addressing both the delays in reaching and receiving care, and subsequently preventing maternal mortality and morbidity.
Each component of the HS model addresses different elements of the three-delay model, providing an efficient and effective approach to the delivery of maternal healthcare and maternal education in resource-poor settings. With the successful implementation of the HS model, MAA aims to improve maternal and neonatal health outcomes in Bangladesh.
Copyright Maternal Aid Association 2023. UK Registered Charity 1166021
Fill in your details and stay up to date with our latest news